Connect With Us
Blog
Items filtered by date: March 2022
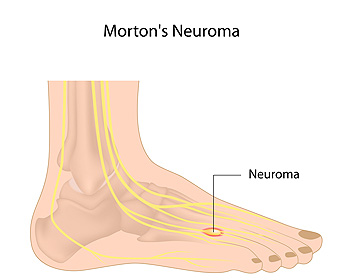
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Stretches That May Relieve Pain from Morton Neuroma
 The nerve tissue between the third and fourth toes are affected when a condition known as Morton’s neuroma is present. It can cause significant pain, and some people say it feels as if there is a rock or pebble inside the ball of the foot. The most common pain consists of a stabbing or burning sensation that typically worsens over time. This condition can develop as a result from wearing shoes that are too narrow or from medical conditions like bunions, hammertoes, and flat feet. Mild relief may be found when the affected foot is elevated or massaged. It can also be beneficial to perform certain exercises to maintain and strengthen the arch of the foot. Fill a plastic bottle with ice and roll it back and forth along the bottom of the foot. (This will help with inflammation too) Another stretch can be performed while sitting down with your legs straight in front of you. Place the ball of your foot in the middle of a towel, then grab both ends of the towel and gently pull towards your shin. If you have pain in the ball of your foot, please schedule an appointment with a podiatrist who can properly diagnose and treat Morton’s neuroma.
The nerve tissue between the third and fourth toes are affected when a condition known as Morton’s neuroma is present. It can cause significant pain, and some people say it feels as if there is a rock or pebble inside the ball of the foot. The most common pain consists of a stabbing or burning sensation that typically worsens over time. This condition can develop as a result from wearing shoes that are too narrow or from medical conditions like bunions, hammertoes, and flat feet. Mild relief may be found when the affected foot is elevated or massaged. It can also be beneficial to perform certain exercises to maintain and strengthen the arch of the foot. Fill a plastic bottle with ice and roll it back and forth along the bottom of the foot. (This will help with inflammation too) Another stretch can be performed while sitting down with your legs straight in front of you. Place the ball of your foot in the middle of a towel, then grab both ends of the towel and gently pull towards your shin. If you have pain in the ball of your foot, please schedule an appointment with a podiatrist who can properly diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr.Kitana of practice KB3. ourdoctor Joomla 3 will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact ouroffice Joomla 3 located in Contact Us TAG . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Morton's NeuromaToenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
What Causes a Toenail Infection?
Onychomycosis is the medical term for a fungal nail infection. Onychomycosis can occur in both fingernails and toenails; however, it occurs more commonly in toenails. This infection can cause your toenails to become discolored, hardened, brittle, crumbled, thickened, and distorted. In some cases, the infection can even spread to the surrounding skin making it red, cracked, swollen or itchy. The fungal organisms that cause onychomycosis love warm, moist, and dark places, which is why it is wise to keep your feet clean and dry. You should never share personal items like towels, shoes, or nail clippers, and avoid going barefoot in locker rooms, communal showers, and public pool areas. Also, if you get your nails done in a salon, make sure they sterilize their equipment properly. Toenail infections can be difficult to treat at home since they can get deep into the layers of the nail, or even underneath the nail. A podiatrist can offer a variety of professional treatments for toenail infections, including prescription topical and oral medicines, laser therapy, or even debridement.
For more information about treatment, contact Dr.Kitana of practice KB3. ourdoctor Joomla 3 can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact ouroffice Joomla 3 located in Contact Us TAG . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Read more about Toenail FungusJoint Replacement Surgery
When conservative, noninvasive treatments prove unsuccessful, podiatrists will often turn to surgery as the last line of treatment for their patients. If patients are suffering from joint pain, issues in mobility, or are seeking to correct a deformity, joint replacement surgery is an effective option. Joint replacement surgery is also successful in treating arthritis, which is the most common cause of improperly working joints.
Patients with symptoms that include joint pain, stiffness, limping, muscle weakness, limited motion, and swelling are typically considered for joint replacement surgery. Range of motion and activity post-surgery will vary between patients and depending on the specific surgery performed, the affected joint, and the damage that will need to be repaired.
Joint replacement surgery replaces the damaged cartilage and bone, the latter if required. The damaged cartilage is typically replaced with a prosthesis that is attached to the bone, allowing the implant to grow into the bone. Following surgery, the patient will typically undergo physical therapy to become familiar with movement using the replaced joint.
Ankle Replacement Surgery
When your ankle joint is damaged by arthritis, trauma, or a medical condition and it’s not responding to conservative treatment—and your quality of life is suffering—ankle replacement surgery may offer relief. This may be a viable treatment option, depending on your condition and overall health. Ankle replacement surgery (sometimes referred to as ankle arthroplasty) involves removing the damaged bone and cartilage of the ankle joint and replacing them with prosthetics made of metal or plastic that work together and operate like your natural ankle joint. Ankle replacement surgery can help increase stability and mobility in the joint as well as reduce pain. To learn more about ankle replacement surgery and determine if you might be a good candidate, it is a good idea to consult with a podiatrist for an exam and diagnosis.
In certain cases, in which the patient suffers from extreme pain or damage in a joint, joint replacement surgery may be deemed useful. If you have constant pain in a foot joint, consult with Dr.Kitana from practice KB3. ourdoctor Joomla 3 will assess your condition and provide you with quality foot and ankle treatment.
What Is Joint Replacement Surgery?
Over time, joints wear down; this can be exacerbated by diseases and conditions. Joint replacement surgery, also known as arthroplasty, is when a damaged joint is surgically removed and replaced with a prosthesis. Prostheses, which can be made of ceramic, plastic, or metal, act as joints in lieu of an actual joint. One of the most prevalent causes for joint replacement is arthritis.
Arthritis in the Foot
Arthritis can occur in any joint in the body, including in the feet. Common types of arthritis in the foot are osteoarthritis, rheumatoid arthritis, and gout. The big toe is usually where arthritis occurs in the foot; this is known as hallux rigidus.
Joint Replacement Surgery in the Foot
The most common form of joint replacement in the foot is a first metatarsophalangeal (MTP) joint placement. MTP joint replacement surgery is designed to treat hallux rigidus. Surgery is not intensive, and recovery occurs within one to two months after the procedure has been done. Overall, joint replacement surgery is a safe and effective way to treat pain in the joint of the foot.
If you have any questions, please feel free to contact ouroffice Joomla 3 located in Contact Us TAG . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Joint Replacement SurgeryVascular Testing in Podiatry
In foot care, vascular testing may be required in the diagnosing and treatment of certain podiatric conditions. Vascular testing is particularly relevant for patients with high-risk diabetes, poor circulation, peripheral artery disease (PAD), and chronic venous insufficiency (CVI). Procedures typically involve the examination of blood vessels throughout the body for blockages or buildup.
Vascular testing is very important for the diagnosis of various conditions, including peripheral artery disease and chronic venous insufficiency, as these conditions can greatly affect one’s quality of life and cause pain in the lower limbs. Circulatory problems in the feet and ankles can reflect issues throughout the body, making testing of the blood vessels pertinent.
Testing methods vary between practitioners and can be specific to certain foot and ankle problems. Modern technology has brought about the ability to perform vascular testing using non-invasive methods, such as the cuff-based PADnet testing device. This device records the Ankle-Brachial Index (ABI)/Toe-Brachial Index (TBI) values and Pulse Volume Recording (PVR) waveforms. Contact your podiatrist to determine what vascular testing is available for your needs.
Why Is Duplex Ultrasound Used to Diagnose PAD?
If your podiatrist suspects that you may have peripheral artery disease (PAD), they will most likely perform a vascular test called a duplex ultrasound. Duplex ultrasound uses two modes of ultrasound: 1) traditional ultrasound to create images of your blood vessels based on sound waves bouncing off them, and 2) doppler ultrasound to estimate the speed and direction of blood by recording sound waves that reflect off it as it flows. Duplex ultrasound is non-invasive and painless. Your podiatrist will spread gel on the skin of the area(s) to be tested, and then wave a transducer wand which emits the sound waves and records the echoes that are reflected. For more information about duplex ultrasound, ask your podiatrist.
Vascular testing plays an important part in diagnosing disease like peripheral artery disease. If you have symptoms of peripheral artery disease, or diabetes, consult with Dr.Kitana from practice new. ourdoctor Joomla 3 will assess your condition and provide you with quality foot and ankle treatment.
What Is Vascular Testing?
Vascular testing checks for how well blood circulation is in the veins and arteries. This is most often done to determine and treat a patient for peripheral artery disease (PAD), stroke, and aneurysms. Podiatrists utilize vascular testing when a patient has symptoms of PAD or if they believe they might. If a patient has diabetes, a podiatrist may determine a vascular test to be prudent to check for poor blood circulation.
How Is it Conducted?
Most forms of vascular testing are non-invasive. Podiatrists will first conduct a visual inspection for any wounds, discoloration, and any abnormal signs prior to a vascular test.
The most common tests include:
- Ankle-Brachial Index (ABI) examination
- Doppler examination
- Pedal pulses
These tests are safe, painless, and easy to do. Once finished, the podiatrist can then provide a diagnosis and the best course for treatment.
If you have any questions, please feel free to contact ouroffice Joomla 3 located in Contact Us TAG . We offer the newest diagnostic and treatment technologies for all your foot care needs.